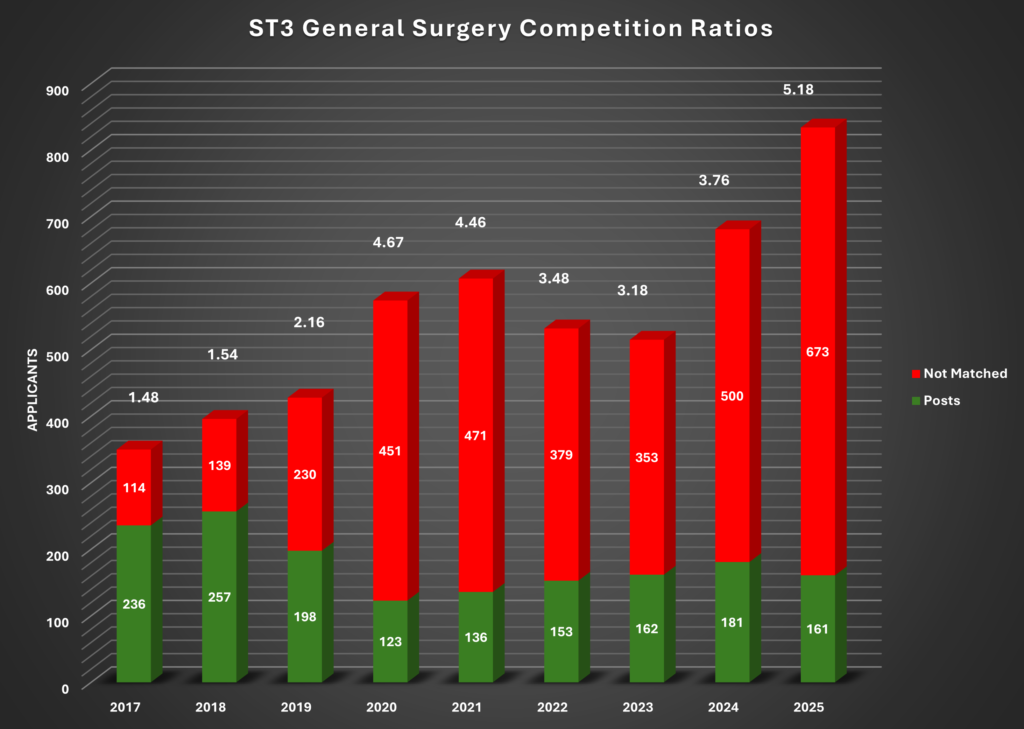
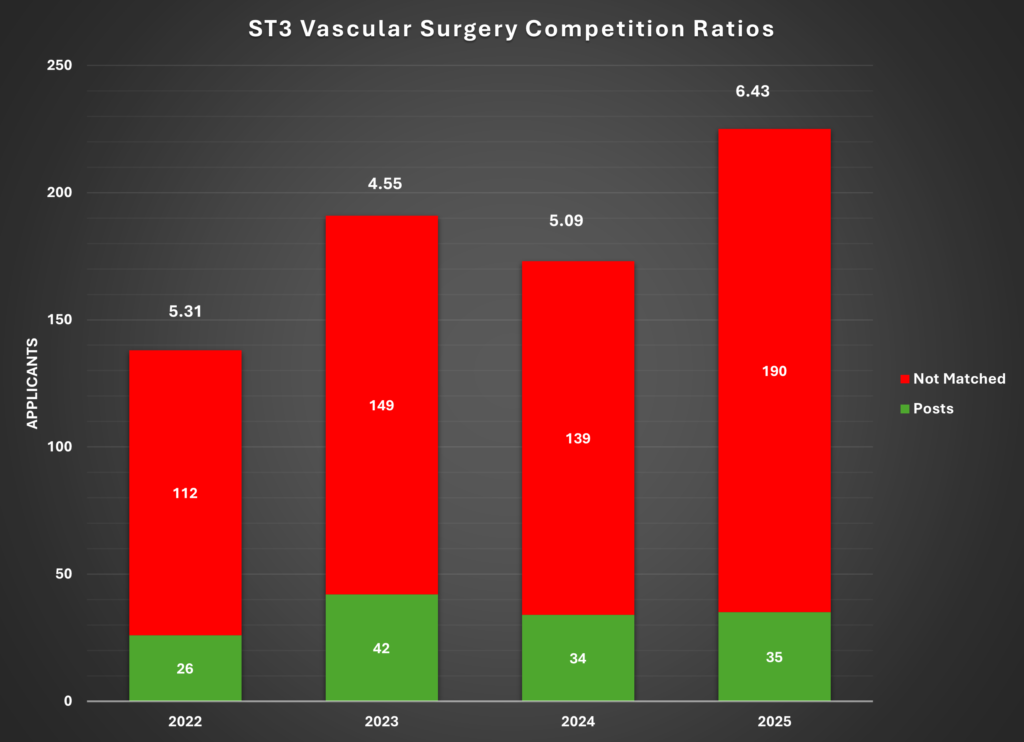
Getting National Training Number (NTN) in General Surgery and Vascular Surgery Speciality ST3 post is becoming highly competitive. ST3 Portfolio Contents + Interview performance are the only opportunities in the year to present the best of yourself. Intelligent preparation is the key.
Please note there will be separate application and interview for General and Vascular Surgery for 2026 recruitment as has been the case in last few years. Self assessment criteria and interview patterns also also different for General and Vascular Surgery. Those keen to apply for both General and Vascular Surgery are required to submit two separate applications.
Following is snapshot of General Surgery / Vascular Surgery ST3 Interview Competition Ratios over last few years
Here at traineeportal.co.uk we have teamed up with experts in interview preparation and successful candidates to give you the best possible advice on how to prepare for your ST3 General Surgery / Vascular Surgery portfolio and interview. We have compiled questions bank in consultation with previous successful candidates, and have team of experts to help you with portfolio and interview preparation.
Successful training interview outcome requires sound preparation. It involves techniques along with knowledge of the subject. Knowing precisely what the interviewer wants, and presenting them exactly what is needed is the secret to successful interview. Here at traineeportal.co.uk we will tell you exactly how to prepare for your ST3 Interview.
First of all! Start early. Don’t leave anything for end as you will keep improving upon your preparation as you go along. Don’t forget to give thorough read to applicant guide by JCST and HEE. A copy of 2026 applicant guide for General Surgery can be downloaded from following links.
Vascular surgery ST3 Application guidance can also be viewed online at HEE website: https://medical.hee.nhs.uk/medical-training-recruitment/medical-specialty-training/surgery/higher-surgery/vascular-surgery
Also go through ST3 General Surgery Person Specifications 2026 and ST3 Vascular Surgery Person Specifications 2026 to have good insight of what is required and what is desirable.
Please note GMC Registration in mandatory to apply for 2026 round.
Application Timeline 2026
| Activity | Date(s) |
| Applications open | At 10am, Thursday 20 November 2025 |
| Applications close | At 4pm, Thursday 11 December 2025 |
| Evidence Verification / Upload | Dec 16, 2025 – Jan 12, 2026 (GS) Dec 12, 2025 – Dec 19, 2025 (VS) |
| Interview Invite | By Tuesday March 10, 2026 (GS) |
| Interview dates | March 26-27, 2026 (General Surgery) |
| February 9, 2026 (Vascular Surgery) | |
| Interview venue | Remote interview (Qpercom Recuit) |
| Initial offers released all regions | 5pm, Tuesday 14 April 2026 |
| Hold deadline | At 1pm, Wednesday 22 April 2026 |
| Upgrading deadline | At 4pm, Thursday 23 April 2026 |
| Hierarchical Deadline | At 4pm, Tuesday 06 May 2025 |
| Training start date | August/October 2026 (TBC by employing trust) |
Eligibility Criteria / Long Listing
• MBBS or other equivalent medical qualification.
• Successful completion of MRCS by day after results for May 2026 examination diet
are released
• Full GMC registration at time of application and hold a current licence to
practise at the time of appointment.
• Evidence of achievement of CT/ST1 competences in core surgery at time of application &
CT/ST2 competences in core surgery by time of appointment.
• Eligibility to work in the UK.
• Not previously relinquished, released or removed from a training programme in this
specialty except under exceptional circumstances.
• Fitness to practise.
• Sufficient language skills (e.g. IELTS).
• Ability to provide a complete employment history.
Not already hold, nor be eligible to hold, a CCT/CESR in the specialty they are applying for and/or must not currently be eligible for the specialist register for the specialty to which they are applying
Core Competences for IMGs
Those who do not have Core Surgical Training in UK, they need to get their competencies signed off by the consultants.
Certificate of Readiness to Enter Higher Surgical Training (Previously known as Alternative Certificate of Core Competence) can be downloaded as below for your review.
The CREHST form is update for 2026 application – it can be downloaded via the link below.
Short Listing
Due to increasing number of candidates and interviewing capacity, short listing will be performed in 2026 as has been the case in last few years. Short listing procedure is different for General Surgery and Vascular Surgery.
For General Surgery: score will be calculated by the panel after reviewed your evidence which should be verified by the Educational Supervisor or equivalent and evidence submitted.
For Vascular Surgeyr: as part of the Oriel application form you will be asked to provide a self-assessment score depending on your personal achievements. Your total self-assessment score will be used for shortlisting purposes.
You will be later required to upload evidences to support your selection to the self-assessment portal. Uploaded evidence will be reviewed and scored by the assessors. Scores will be provided to applicants. Applicants unhappy with the score given can request a review by another assessor in line with the policy in place. No new evidence can be submitted for the review.
In line with interview capacity, shortlisted candidates with the highest scores will be invited to attend a remote interview. Interview capacity for General Surgery is 288 and for Vascular Surgery it is 96.
Self – Assessment Scoring:
Self scoring criteria is different for General and Vascular Surgery for 2026 applications
General Surgery Scoring:
Listed below are the 7 questions which appear on the 2026 General Surgery ST3 application form along with the possible responses to each question and details of suitable evidence to substantiate your responses. A guide to the scoring for each question is provided, with descriptions of the quality
indicators where appropriate.
Applicants must record their responses to all 7 questions using the following templates.
Along with evidences, candidates are required to submit following checklist signed by the Educational Supervisor or Equivalent.
General Surgery ST3 Shortlisting Evidence Applicant & Educational Supervisor Checklist
After filling out the 7 templates with your responses, applicants must upload their templates, with supporting evidence to the Evidence Upload Portal.
For each question a description of the evidence required is given. You will only be awarded marks if the evidence provided matches the description of the evidence required for that domain.
Maintaining trust by being open and honest and acting with integrity is one of the key elements of Duties of a Doctor (GMC). If it is subsequently discovered that any statement made on your application is false or misleading, evidence will be collected, and you may be referred to a Probity
Panel.
Maximum Total Score: 60
A breakdown of weightage of each domain is as follows.
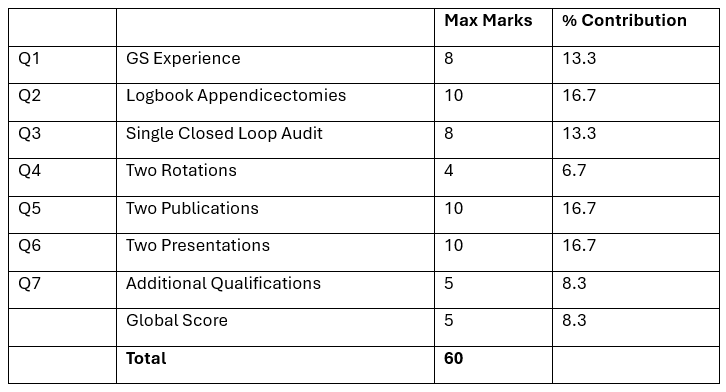
Question 1 – General Surgery Experience: (Maximum Score: 8 -> 13.3%)
By the end of July 2026, or by the completion of Core Training if this is later, how many months full time (or equivalent if LTFT) will you have spent in total in General Surgery in any Post-Foundation job in any country? Eligible posts must include experience in both unselected emergency general surgery and elective general surgery (or a recognised general surgical sub-specialty) Please do not include any other posts.
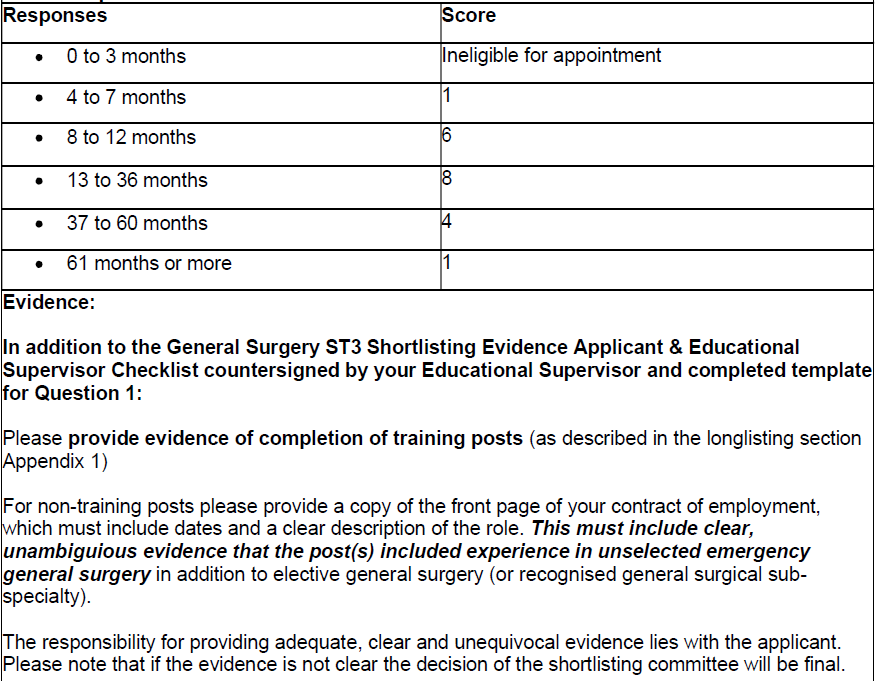
- For non-training posts please provide a copy of the front page of your contract of employment, which must include dates and a clear description of the role
- If the front page of your contract does not include both start and finish dates other evidence will be required to confirm the duration of post e.g. Letter from HR/Head of Service/Supervising Consultant
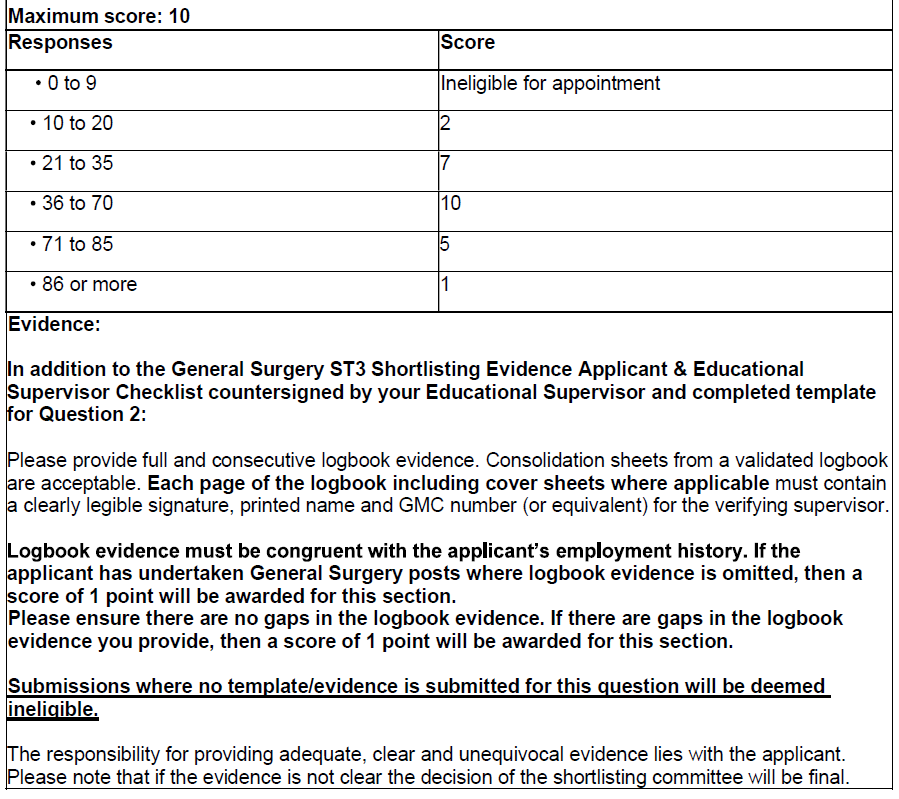
Question 2 – Surgical Experience – Appendicectomies: (Maximum Score: 4 – 6.7%)
By the time your evidence is submitted, how many appendicectomies (laparoscopic and/or open) have you completed? Do not include cases where your role was limited to assisting the operating surgeon only.
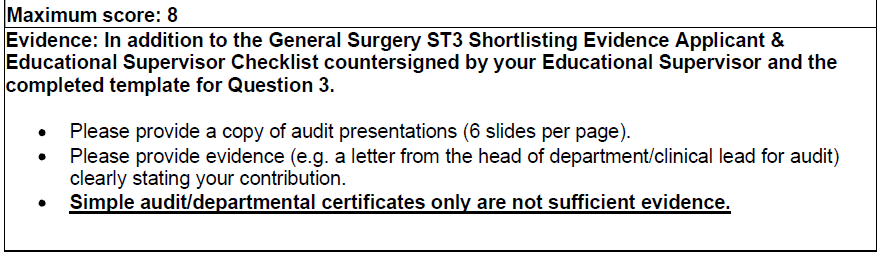
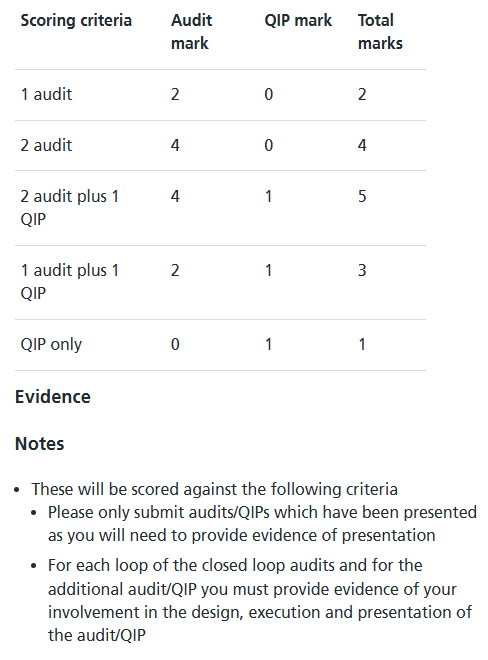
Question 3 – Single Best Closed Loop Audit: (Maximum Score: 8 -> 13.3%)
Please submit your single best closed loop audit. Please only submit an audit which has been presented, as you will need to provide evidence for this. For each loop of the closed loop audit you must provide evidence of your involvement in the design, execution and presentation stages.
Points will be awarded for e.g. depth of candidate involvement, reference standard, study design, importance of clinical question and impact of work.
Applicants should note that to qualify as a closed-loop audit, there must be clear evidence of applicant involvement in both audit cycles. Submissions where the applicant is deemed by the short listers to have only been involved in the initial or re-audit will receive zero points and are ineligible to proceed to the interview stage.
Applicants should also note that very generic audits are no longer accepted e.g. (Mandatory) Trust VTE audits, antibiotic prescribing compliance, simple casenote/operation note audits, as these are felt to have low/no value in discriminating between the best applicants for ST3.
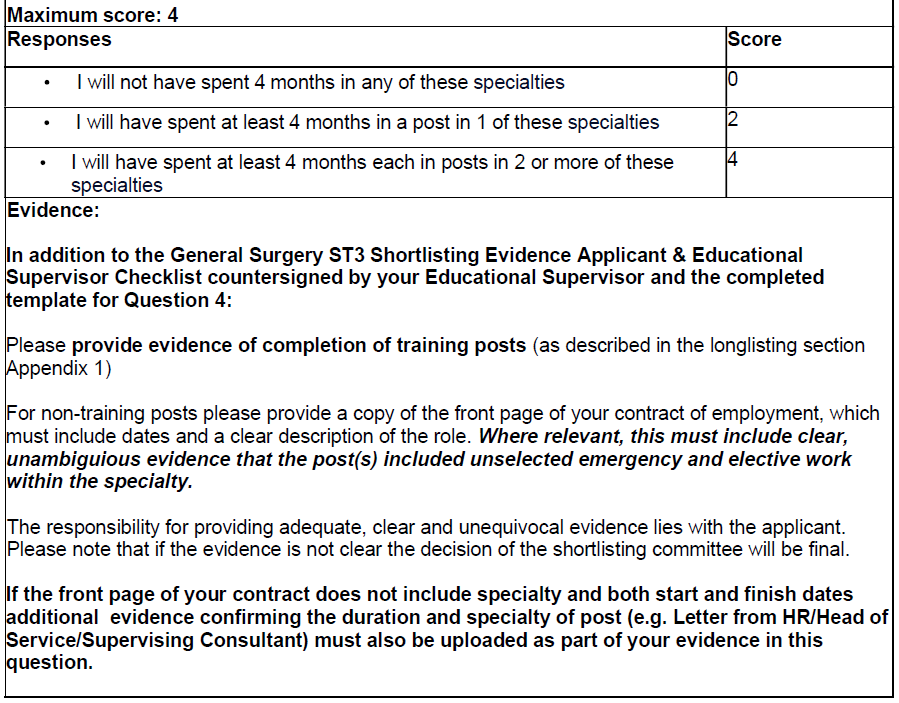
Question 4 – Rotations: (Maximum Score: 4 -> 6.7%)
By the end of July 2026, or the completion of Core Training, will you have spent at least 4 months in T&O, Plastic Surgery, Neurosurgery, ENT Surgery, Cardiac/Thoracic surgery, A&E, ITU, Paediatric Surgery, Urology, Vascular or OMFS posts since completing your Foundation Programme?
In order to be eligible for points, applicants must evidence that they have completed a minimum of 4 months full time (or equivalent if LTFT) in both unselected emergency and elective work within the relevant specialty.
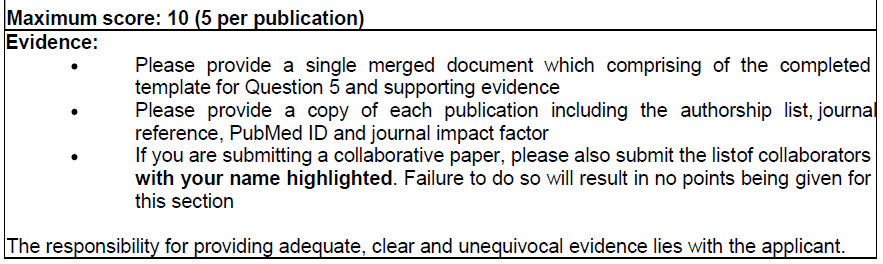
Question 5 – Publicaitons: (Maximum Score: 10 (5+5) -> 16.7%)
Please submit your 2 best publications, published in a PubMed indexed journal. In order to be eligible for this section, publications must have a PubMed ID, journal impact factor, and be published by the time your evidence is submitted.
Irrespective of PubMed ID, publications in pay-to-publish model journals (e.g. Cureus) are no longer be accepted and will score 0 points.
Please submit in order of preference, with your best publication first. Do not include articles which have not yet been published. Collaborative papers, abstracts, case reports, letters or technical tips are acceptable. Points will be awarded for candidate contribution, level of authorship, quality of study and impact factor of publication.
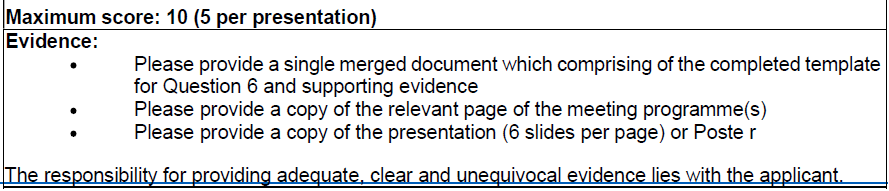
Question 6 – Presentations: (Maximum Score: 10 (5+5) -> 16.7%)
Please submit your 2 best academic presentations. In order to be eligible for this section, the presentation must have been published by the time your evidence is submitted.
Please submit in order of preference, with your best presentation first.
You may include poster presentations.
In event that the presentations duplicate/repeat one another (e.g. results/conclusions are the same and/or derived from the same data analysis), only the first presentation will be scored.
Points will be awarded for e.g. depth of candidate contribution, being the presenter of the work, quality of study.
Applicants should note that presentations made at departmental/hospital/regional (or equivalent) level only are not eligible. Decisions regarding benchmarking of the relative level of a scientific meeting are at the discretion of the shortlisting panel/clinical leads irrespective of meeting title.
Applicants should note that presentations made in the course of the applicant delivering teaching/training activity are not accepted. This category of activity can be discussed during the professional development interview station.
Question 7 – Additional Qualifications: (Maximum Score: 5 – 8.3%)
By the time your evidence is submitted, have you been awarded a stand-alone degree by a UK university (see evidence below)? (NB: This does not include intercalated degrees, including intercalated degrees which are part of a standard training programme).
Scoring does not include intercalated degrees, including those which are recognised to be a mandatory component of a postgraduate training programme, either in the UK or overseas. If uncertain please refer to the following publication: https://doi.org/10.1308/rcsann.2024.0086
This category has now been broadened to include PG Certs, Diplomas and taught Masters degrees. Points will not be awarded unless evidence is provided that the qualification has been awarded.
Vascular Surgery Self Assessment Scoring:
Criteria for 2026 Application Self Assessment score is as follows, please note there are minor changes each year.
Listed below are the 9 Self-Assessment questions that appear on the application form along with the possible responses to each question and details of suitable evidence to substantiate your responses.
If the interviewers are unable to verify that your evidence matches the answers you provided on your application form, you will not be awarded any marks for those criteria.
If it is subsequently discovered that any statement is false or misleading, evidence will be collected, and you may be referred to a Probity Panel.
Please note all time periods specified in the Self-Assessment Form refer to full-time equivalent.
Achievements within last 10 years of Dec 11, 2025 for 2026 application.
If an achievement legitimately may fit under multiple domains, it is valid to claim in both categories (for example, academic work which was presented orally then subsequently published).
Completed Achievements only at time of submission
The Maximum achievable self-assessed score is 39.
Interview Capacity: 96
Distribution of Marks across different Domains
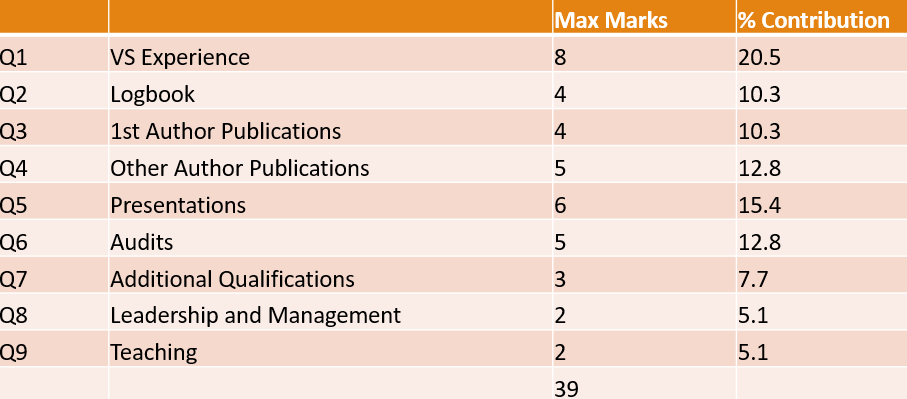
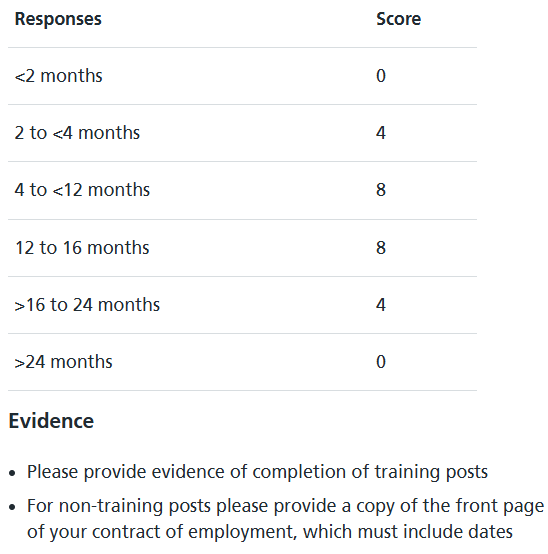
Domain 1: Vascular Surgery Experience: (Max Score 8 -> 20.5%)
By the end of September 2026, how many months (whole time equivalent) will you have spent after medical school in total in Vascular Surgery in any country? Please do not include any other posts.
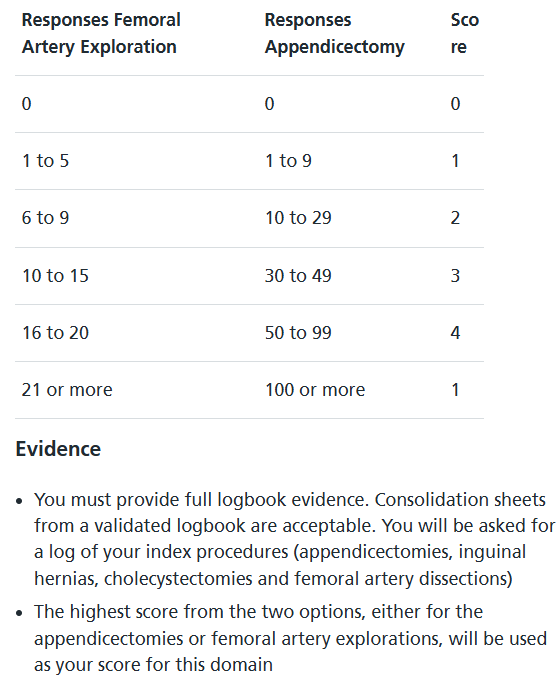
Domain 2 – Surgical Experience (Appendicectomies / Femoral Explorations): (Max Score: 4 -> 10.3%)
At the time of application, how many appendicectomies (laparoscopic and/or open) or femoral artery dissections have you completed which have been done either STS or STU or P or T?
The higher of the two scores will count. These must be recorded in a validated logbook.
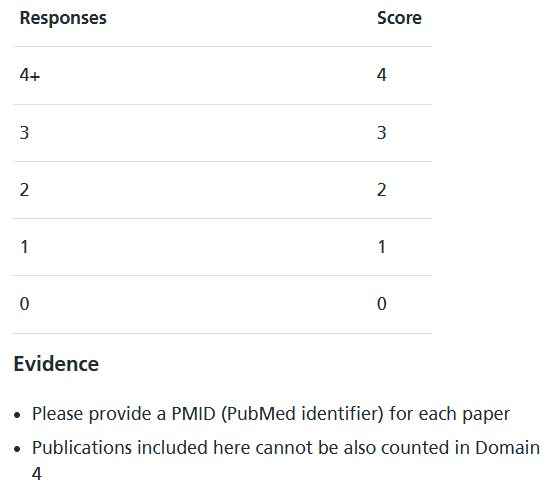
Domain 3 – First Author Publications : (Maximum Score: 4 -> 10.3%)
At the time of application, how many First author publications have you had published in any PubMed indexed journals? Do not include published abstracts, case reports, letters or technical tips.
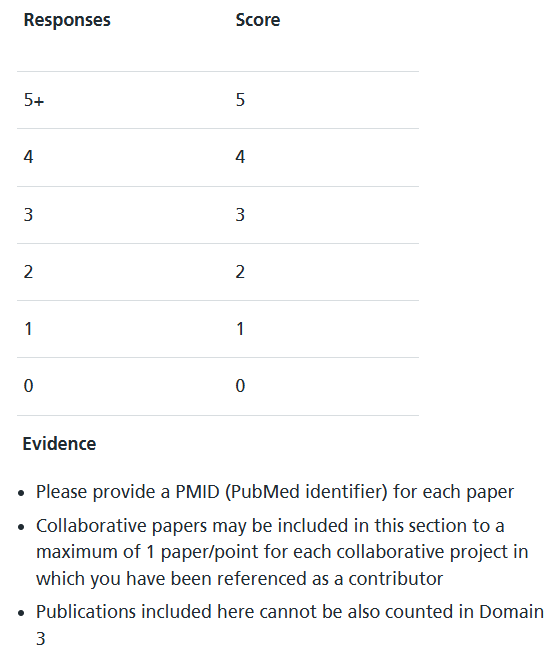
Domain 4 – Other Publications: (Maximum Score: 5 -> 12.8%)
At the time of application, how many other publications have you had published in any PubMed indexed journals? Do not include published abstracts, case reports, letters or technical tips.
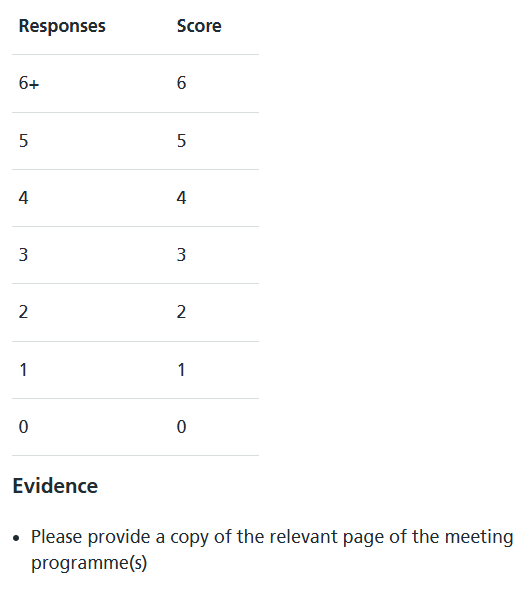
Domain 5 – Presentations: (Maximum Score: 6 -> 15.4%)
At the time of application, and in the last two years whole-time equivalent (WTE) of clinical practice how many national and international presentations have been given of work in which you are a listed author? Do not include poster presentations.
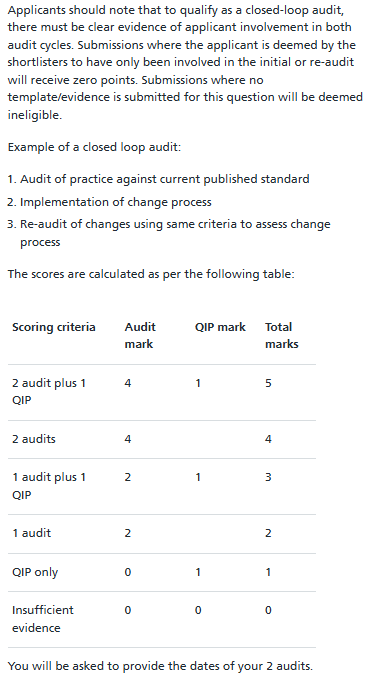
Domain 6 – Audits / QIPs: (Maximum Score: 5 -> 12.8%)
Please submit your 2 best closed loop audits and your best additional audit or Quality Improvement Project that have resulted in a departmental presentation of the results at the time of application.
Audits must be at least a full loop (a full audit cycles that involves a second audit following an implemented change) and compared to a published clinical standard.
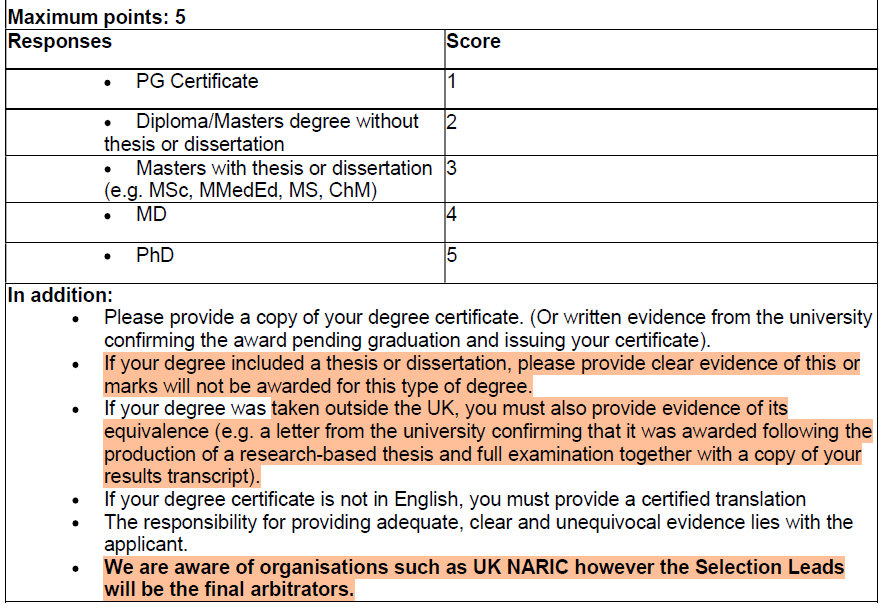
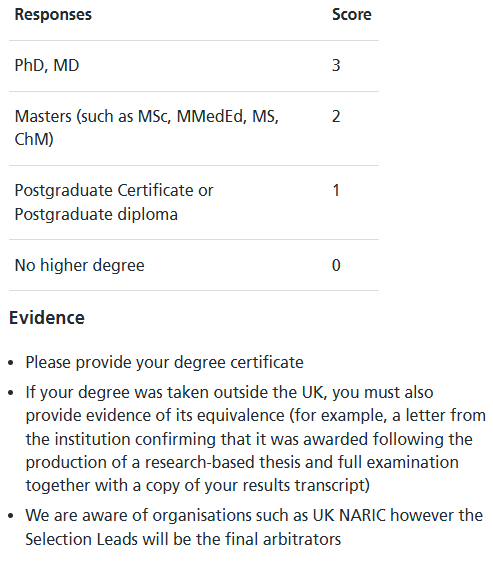
Domain 7 – Additional Qualifications: (Maximum Score: 3 -> 7.7%)
At the time of application, have you completed and been awarded a stand-alone higher degree or equivalent (see evidence below) examined by thesis/dissertation? (NB: This does not include intercalated degrees or primary medical degrees).
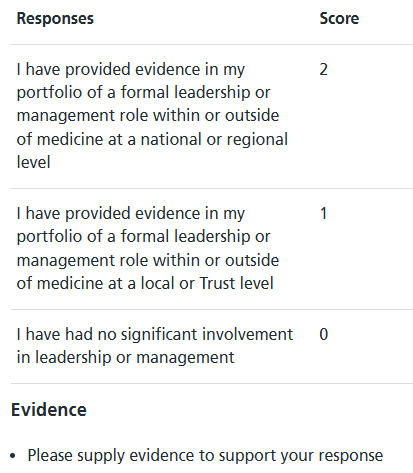
Domain 8 – Leadership and Management: (Maximum Score: 2 – 5.1%)
Please select one statement that best describes your involvement in leadership or management in the last two years whole-time equivalent (WTE) of clinical practice.
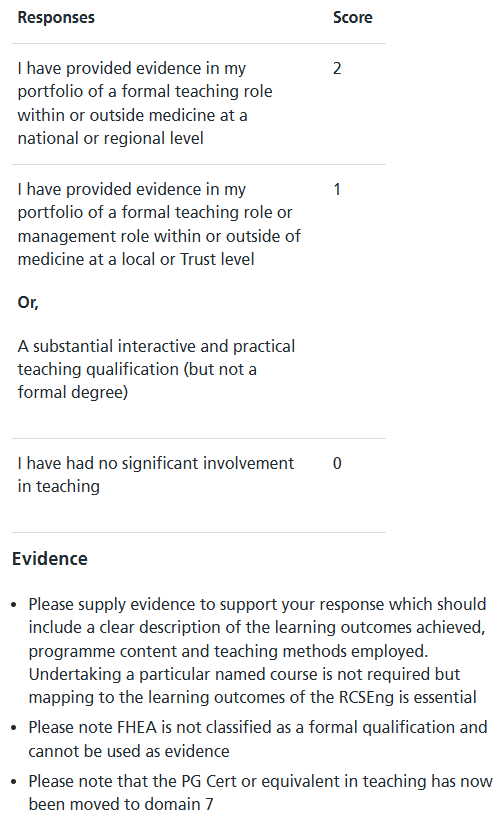
Domain 9 – Medical Education / Teaching: (Maximum Score: 2 – 5.1%).
Please select one statement that best describes your involvement in medical education/teaching in the last two years whole-time equivalent (WTE) of clinical practice.
ST3 General Surgery / Vascular Surgery Interview Format
There will be separate interview of General Surgery and Vascular Surgery.
Before you attend the interview it is very important that you have prepared properly. The interview for 2026 induction will be conducted online via QPERCOM. It will be a total of approximately 40 minutes interview (Approximately 50 minutes for Vascular Surgery). Interviewers panel will comprise of 2 consultants (4 Consultants in Vascular Interview). There may be an observer who will not be assessing candidates. This may be the Lay Representative who is there in an independent role to assist in the quality assurance of the interview process, or a Consultant who is present to observe and assess the interviewers. Senior trainees are also invited to attend to observe. They play no part in the assessment. There will be a maximum of one observer present at any time.
The interview will be split into the following sections:
➢ Clinical & Management scenarios reading time (5 minutes)
You will be given two scenarios and have 5 minutes reading time prior to the interview– one scenario will be clinical about a patient, and one will be a management scenario about a problem based in the clinical environment.
➢ Clinical scenario & questions (10 minutes)
You will have 10 minutes to answer questions about the clinical scenario and other related questions.
➢ Management scenario & questions (10 minutes)
You will have 10 minutes to answer questions about the management scenario and other related questions.
➢ Professional Development questions (10 minutes) – (General Surgery Only)
You will have 10 minutes to answer questions about aspects of your career to date.
➢ Communication Scenario and Questions (10 minutes) – (Vascular Surgery Only)
You will have 5 minutes to answer questions about the communication scenario and other related questions.
➢ Virtual Skills Scenario and Questions (10 minutes) – (Vascular Surgery Only)
You will have 10 minutes to answer questions about a virtual operative skills scenario and other related questions.
General Tips for All Stations:
- Remain Calm
- Understand the questions before jumping on to answer
- Structure your answers
- Keep the answers to the point
- Examiners are also pressed for time as they need to complete the questions they have within given time, don’t take it negative if they stop you and ask next question. That would probably mean that they have got the answer they were looking for
- Look for hidden / obvious clues
Portfolio Station
At this station your portfolio will be reviewed in order to assess your level of achievement. You will be scored against a set of defined descriptors that have been carefully developed to assess your achievements against the criteria set out in the nationally agreed person specification.
You should be prepared to answer following questions related to your portfolio at the time of interview.
Question 1 – Is there anything that you have added to your portfolio since the application that you would like to tell us about?
Question 2 – What else in your portfolio exemplifies your commitment and suitability to a career in surgery?
Question 3 – What are you most proud of in your portfolio and why?
There will be further questions related to leadership and teaching aspects of the portfolio.
Clinical And Management Station
At this station you will be given two scenarios and will have 5 minutes reading time – one scenario will be clinical about a patient, and one will be a management scenario about a problem based in the clinical environment. You will then have 20 minutes with the interviewers who will spend half of the time (10 minutes) on each scenario.
Clinical Scenario:
Clinical Scenario will be about every day clinical situations and focus of this scenario will mainly be the clinical knowledge and approach. There will be some component of management also but primary focus would remain clinical.
Management Scenario:
This scenario will be about commonly encountered management issues in clinical environment. There will be clinical component but primary focus of this scenario will be management and organisational skills.
A comprehensive mnemonic to attempt these scenarios is SPIES.
S: Situation / Issues: Identify all the possible issues in the scenarios. Like clinical, organizational and training issues.
P: Priority: Priorize the issues identified. Clinical / Patient safety should always take priority.
I: Intervention: How will you intervene? In many situation you will start by gathering further information. In management scenarios particularly you will frequently need to incorporate audit cycle. (Plan – Do – Study – Act)
E: Escalate: Escalate to those concerned. For example clinical supervisor, educational supervisor, programme director, clinical lead, medical director, nursing incharge…
S: Support: Support the staff, juniors, colleagues and seniors in the intervention and the change you plan.
Professional Communications Station (Vascular Only)
In this section you will be provided with clinical information to read about a number of patients. You will then be required to make a telephone call to an interviewer acting as a consultant on the other end of the call. Your approach to this task will be scored against criteria set out in the nationally agreed person specification. You will be scored for your professional way of communication, prioritisation, picking up urgency, appropriate management plan including plan of further investigations.
The total time for this station is 15-20 minutes during which you have to read the scenario, look at the investigations and complete a telephone call to your consultant (Mr/Miss White) – you have 5 minutes to read the scenario and 10-15 minutes for phone call. You will be informed when the time allocated for the call is at the halfway point, and again 1 minute from the end.
Traineeportal Perks to attempt professional communications station:
Common scenarios are a call to consultant after the shift, after post-take ward round or after you are done with clinic. Uncommonly a call to the radiologist to discuss patients for possible further radiological investigation or intervention can also be expected.
As you go through the scenarios in the initial 5 minutes, make a grid on the paper to give you quick summery of which patients are critical and which are non urgent. Or in case of outpatient clinic scenarios, patients requiring admission, further investigation / referral to other speciality / booked for elective surgery, or discharge.
Write numbers in a column to represent the given patients. (Patients are numbered already). Then you can use star scheme from 1 to 3 to give you an idea of which patients are most critical and which are the least.
In case of call after clinic, you can give 3 stars to the patients you have admitted, 2 stars for further investigation / referral to other speciality / booking for elective surgery, 1 star to those you plan to be discharged back to GP.
Ready for the call!
- Confirm who you are speaking to (Good Morning, Am I speaking to Mr White?)
- Introduce yourself and your role (Hello, I am …. ST3 registrar on call)
- Ask if it is ok to talk through patients
- Give a summery first. (Something like: I have seen 9 patients on call. There are two patients who need urgent operation, three patients I am concerned about, there are two stable admissions, one to be discharged and one to be referred to urology.)
- Then talk through patients one by one in the order of priority
- Don’t read out what is written on the sheet, give brief presentation and your clinical impression
- Always describe what is next step (further investigation / resuscitation / admission / opinion from other specialities etc, For example in a female patient with clinically appendicitis make sure you get urine dip and pregnancy test, patient with biliary colic / cholecystitis make sure you get LFTs, Serum Amylase, Critically ill patients make sure you involve critical outreach team / intensivist.. etc)
Valuable Resources
Following you can download valuable resources to help you preparing frequently asked questions at Clinical and Management stations
Mental Capacity Act – Who decides when you cannot
Children and Young People Consent to Treatment
ST3 General and Vascular Surgery Questions Bank
Click here to access Questions Bank to practice frequently asked Clinical and Management Practice Questions, And Communication Station Scenarios.